Top 5 STI myths busted
About 16% of people will report having an STI in their lifetime. That’s one in six people in Australia!
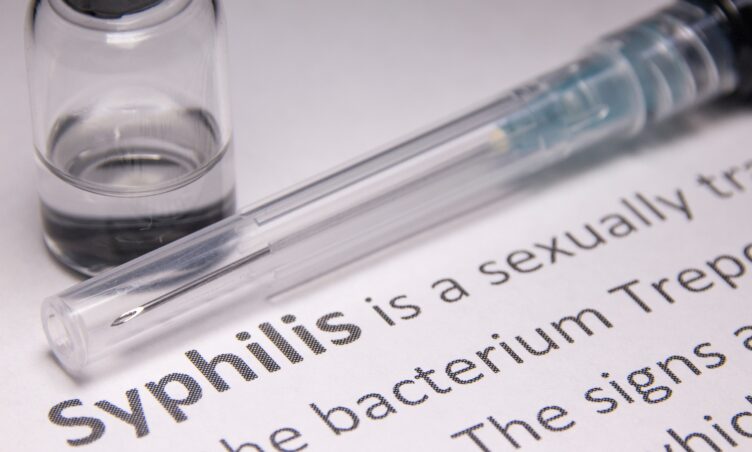
Certain types of STIs have increased in our communities lately, including gonorrhoea (which tripled between 2008 and 2017), and syphilis (which doubled from 2004 to 2017). To keep you as STI-safe as possible, read on as we myth-bust the top five most common misconceptions about STIs with Melbourne doctor, Dr Madeleine.
1. “STIs always show symptoms.”
Symptoms of STIs can include itch, developing a rash or sores on your genitals, unusual discharge and pain passing urine. In people with uteruses, you may experience pain in the lower stomach, and have bleeding after sex or between periods. People with testicles may experience pain in this area.
However, many infections are completely asymptomatic – one study estimated 45% of gonorrhoea cases and 77% of chlamydia cases didn’t present with symptoms! Viruses such as HIV and Hepatitis C often cause infection silently, and can present for the first time years later with life-threatening illness.
As such, it’s important to have STI screening regularly even without symptoms, and to discuss your risk profile with your doctor so you can be tested appropriately. We recommend screening every 6 to 12 months, or more often if you have a new partner or a frequent change in partners.
2. “STIs are only transmitted via penetrative sex.”
STIs can be transmitted with any sexual act! This includes vaginal sex, anal sex, oral sex, and oralanal sex. Sharing toys can also pose a risk. It’s best to protect yourself by using condoms and dental dams whenever you have any type of sex, and keep on top of your own status with regular health checks.
3. “Taking contraception will protect me from STIs.”
Whilst taking some form of contraception is a great idea if you don’t want to become pregnant, it will not protect you from an STI. Ongoing use of condoms or other barrier protection is still essential. And don’t forget that STI protection and contraception are the responsibilities of both partners to think about.
4. “Having an STI means I’m “dirty” or “promiscuous”.”
This is very far from the truth. A person could have sex once and get an STI; alternatively, a person could have multiple partners and remain STI-free by taking appropriate preventative steps. As such, regular screening, abstaining from sex until you’ve been completely treated (such as finishing your course of antibiotics), and making sure any skin sores have completely healed before you have sex again, are very important too.
Also, being aware of language that encourages the stigmatisation of STIs (such as referring to oneself as “clean” from STIs, or implying that STIs only happen to people who have lots of sex with lots of different people), will help us collectively remove the shame associated with STIs, and normalise the need for sexual health care!
5. “Having an STI screen is too expensive for me.”
In Victoria, testing can be bulk-billed or directly-billed – meaning there is no out-of-pocket cost for you to have the test. However, some clinics may charge you to see a GP. If cost is an issue for you, try to find a GP who can bulk-bill you for your appointment or visit a sexual health clinic (as they’re typically free or low cost). You can contact 1800 My Options for STI testing services near you!